Hip Abductor Dysfunction
Understanding lateral hip weakness, pain, and instability related to gluteal muscle injuries
Hip abductor dysfunction refers to weakness, injury, or degeneration of the muscles responsible for stabilising the pelvis during walking and standing, particularly the gluteus medius and gluteus minimus. These muscles play a crucial role in maintaining balance and preventing the pelvis from tilting with each step. When the abductors are not functioning properly, patients may experience pain on the side of the hip, difficulty walking, limping (known as a Trendelenburg gait), or reduced stability.
This condition is commonly seen in middle aged to older adults, especially women, and may be caused by tendon tears, muscle atrophy, nerve irritation, or underlying joint conditions such as arthritis or hip dysplasia. In some cases, the dysfunction may mimic other causes of lateral hip pain, such as trochanteric bursitis, making accurate diagnosis essential.
Dr George Awwad provides a comprehensive assessment of hip abductor dysfunction and offers both non-surgical and surgical treatment pathways, depending on the underlying cause and severity of symptoms.
What are the hip abductor muscles and what do they do?
The hip abductor muscles are a group of muscles located on the outer portion of your hip and upper thigh. Their main role is to stabilise the pelvis and move the leg away from the body, a motion known as abduction. They are essential for maintaining balance while walking, standing on one leg, or climbing stairs.
Key Hip Abductor Muscles
1. Gluteus Medius
- Located on the outer surface of the pelvis.
- The primary muscle responsible for hip abduction and stabilisation during walking.
- Prevents the pelvis from dropping on the opposite side when standing on one leg (Trendelenburg function).
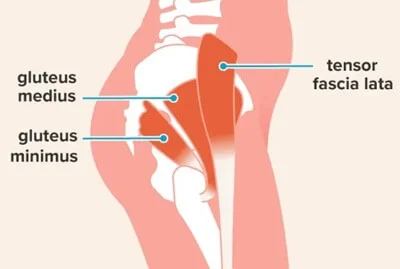
2. Gluteus Minimus
- The smallest and deepest of the gluteal muscles, sitting beneath the gluteus medius.
- Assists in hip abduction and internal rotation.
- Works closely with the gluteus medius to maintain pelvic stability.
3. Tensor Fasciae Latae (TFL)
- A small muscle on the outer thigh that assists with abduction and internal rotation of the hip.
- Connects to the iliotibial (IT) band, contributing to hip and knee movement.
Role in Pelvic Stability and Gait
- These muscles are critical for pelvic alignment and balance during dynamic activities like walking, running, and single-leg standing.
- When functioning properly, the abductors ensure that the pelvis remains level, reducing strain on the lower back and knees.
- If these muscles are weak, torn, or not functioning correctly (as in hip abductor dysfunction), it can lead to a characteristic limping gait (Trendelenburg gait), pain on the outer hip, or instability.
Common causes of hip abductor dysfunction
1. Tendon Tears or Degeneration
- Chronic overuse (e.g. repetitive walking or running)
- Age-related degeneration
- Previous trauma or falls
- Poor biomechanics or compensatory gait patterns
2. Tendinopathy or Inflammation
- Greater trochanteric pain syndrome (GTPS)
- Repetitive strain or overload
- Impaired healing response in older adults
3. Muscle Atrophy or Weakness
- Sedentary lifestyle
- Hip osteoarthritis
- Previous surgery (e.g. hip replacement)
- Neurological conditions such as stroke or nerve injury
4. Nerve Impairment
- Hip or pelvic trauma
- Complications from surgery
- Tumours or mass effect in the pelvic region
5. Biomechanical and Structural Abnormalities
- Hip dysplasia
- Leg length discrepancy
- Pelvic tilt or abnormal gait patterns
- Lumbar spine pathology affecting nerve function or posture
Signs and symptoms of abductor dysfunction
1. Lateral hip pain
- The most common complaint is pain on the outside of the hip, often over the greater trochanter (the bony prominence at the side of your hip).
- This pain may worsen:
- With prolonged standing
- While lying on the affected side
- During activities such as climbing stairs or walking up hills
2. Limping or gait abnormalities
- Weakness in the abductor muscles can lead to a Trendelenburg gait, where the pelvis drops on the opposite side during walking.
- Patients may unconsciously shift their torso over the affected side to compensate, creating a waddling or lurching motion.
3. Muscle weakness
- You may notice difficulty standing on one leg (especially on the affected side), or a sense of instability when walking.
- Climbing stairs, getting up from a chair, or rising from a squat may become more challenging.
4. Tenderness and reduced range of motion
- Pressing on the lateral aspect of the hip often elicits discomfort.
- Some individuals experience stiffness or reduced hip mobility, particularly when trying to move the leg outward or backward.
5. Referred pain
- Pain may radiate down the outside of the thigh or into the buttock.
- It is important to differentiate this from other conditions such as sciatica or hip osteoarthritis.
How hip abductor dysfunction is diagnosed
1. Clinical history
- Your consultation will begin with a detailed discussion of your symptoms, including:
- Activities that aggravate or relieve the discomfort
- Duration of symptoms and any history of trauma or overuse
- Difficulty with daily activities such as walking, climbing stairs, or lying on the affected side
2. Physical examination
- Trendelenburg test: Standing on one leg to check for pelvic drop, which indicates weakness in the gluteus medius.
- Palpation: Tenderness over the greater trochanter may suggest associated bursitis or tendon involvement.
- Strength testing: Manual resistance tests can reveal abductor weakness or pain.
- Gait assessment: Observing your walking pattern helps identify compensatory movements or limping.
3. Imaging tests
- X-rays: Help rule out underlying joint degeneration, fractures, or bony abnormalities.
- Ultrasound: Useful for assessing superficial tendon tears or bursitis.
- MRI: Provides detailed imaging of the hip tendons and muscles and is particularly helpful for detecting partial or full-thickness tears of the gluteus medius or minimus tendons.
4. Diagnostic injection (if needed)
In complex cases, a local anaesthetic and corticosteroid injection into the bursa may help distinguish between bursitis and true abductor tendon pathology. If pain relief is achieved, this may confirm that the pain source is related to bursal inflammation.
Non-surgical treatment options for hip abductor dysfunction
In many cases, hip abductor dysfunction can be managed without surgery, particularly when the condition is caught early or involves partial tendon injury, overuse, or muscular imbalance. The goal of non-surgical management is to reduce pain, restore function, and prevent further deterioration of the hip stabilisers.
1. Physiotherapy and targeted exercise
- Strengthening exercises for the gluteus medius and minimus
- Pelvic stability training to address compensation patterns
- Stretching exercises for surrounding muscles like the iliotibial band and hip flexors
- Gait re-education to reduce strain on weakened abductors
2. Activity modification
- Limiting prolonged walking or standing
- Avoiding stairs or hills where possible
- Changing your sleeping position (e.g. avoiding lying on the affected side)
3. Anti-inflammatory medications
4. Corticosteroid injections
- Reduce inflammation and pain in the surrounding bursa or tendon sheath
- Improve comfort to allow progression with physiotherapy
- Assist in confirming the pain source
5. Shockwave therapy
- Stimulating blood flow
- Promoting healing of the tendon tissue
- Reducing chronic pain
Surgical options for persistent or severe cases
1. Hip abductor tendon repair
- Reattaching the torn gluteus medius and/or minimus tendon to the greater trochanter (outer part of the hip bone)
- Removing any damaged or degenerated tendon tissue
- Anchoring the tendon using sutures or bone anchors
- Open surgery for direct visualisation of the tear
- Minimally invasive (endoscopic or arthroscopic) surgery, where small incisions and a camera are used, potentially reducing recovery time
2. Trochanteric bursectomy
3. Tendon grafting or augmentation
- Reinforce the repair
- Bridge tendon defects that cannot be fully closed
- Provide a scaffold to support tendon healing
