Total Hip Replacement (Arthroplasty)
A Surgical Option for Advanced Hip Arthritis
Total hip replacement, also known as total hip arthroplasty, is a surgical procedure used to relieve pain and restore function in hips affected by severe arthritis, degeneration, or injury. If non-surgical treatments such as physiotherapy, medications, or joint injections no longer provide relief, replacing the damaged hip joint with a prosthetic implant may help improve mobility, reduce discomfort, and enhance your quality of life.
Dr George Awwad performs hip replacement surgery using advanced techniques, including anterior minimally invasive approaches, supported by personalised pre-operative planning. His focus is on achieving precise outcomes and guiding each patient through a well-supported recovery process.
When is hip replacement surgery recommended?
Total hip replacement is typically recommended when the hip joint has been significantly damaged by conditions such as osteoarthritis, rheumatoid arthritis, or past injury, resulting in ongoing pain, stiffness, and reduced function. It is a treatment option considered when non-operative management is no longer effective, and when joint damage begins to interfere with quality of life.
Most patients start with conservative treatments including physiotherapy, anti-inflammatory medications, weight management, and joint injections. These may provide temporary relief, but if symptoms persist or worsen over time, surgery may be discussed as the next step.
Hip replacement may be considered appropriate when:
- Pain interferes with walking, bending, or weight-bearing activity
- Mobility is limited despite physiotherapy or medication
- A walking aid (cane or walker) is increasingly required
- Non-surgical treatment no longer provides lasting relief
- Imaging shows progressive joint degeneration or bone-on-bone contact
Hip replacement is not considered routine or urgent surgery; rather, it is planned when the goal is to restore mobility and reduce discomfort in a joint that is no longer functioning well. The timing of surgery depends on the severity of joint damage, how much your symptoms affect your daily life, and your individual health status.
Dr George Awwad takes a careful and considered approach to this decision. If you’re experiencing ongoing limitations due to hip joint damage, he will guide you through a full assessment and help determine whether surgery may be a reasonable next step in your treatment pathway.

Symptoms that may indicate hip arthritis
Hip arthritis is a degenerative condition that causes inflammation, stiffness, and progressive wear of the hip joint. It is most commonly due to osteoarthritis but may also result from rheumatoid arthritis or previous trauma to the joint. As the cartilage that normally cushions the ball-and-socket joint breaks down, the bones begin to rub directly against each other, leading to pain, reduced movement, and increasing joint dysfunction.
Recognising the signs of hip arthritis
Symptoms of hip arthritis tend to develop gradually. In the early stages, many people notice only occasional discomfort. Over time, symptoms may become more persistent and start to interfere with everyday activity.
Common signs that may indicate hip arthritis include:
-
Pain in the hip or groin area
Often felt deep in the front of the hip or groin, but can also radiate to the thigh, buttock, or knee. -
Stiffness after resting or sitting
Difficulty getting up after sitting for long periods, or morning stiffness that improves with movement. -
Reduced range of motion
Trouble bending, rotating, or spreading the legs may affect tasks like putting on socks or getting in and out of a car. -
Limping or altered gait
Pain may lead to a noticeable limp or changes in walking pattern to avoid putting weight on the affected hip. -
Grinding, clicking, or catching in the joint
These sensations may occur due to joint surface damage or inflammation within the joint. -
Pain worsened by activity and relieved with rest
Walking, climbing stairs, or prolonged standing may aggravate symptoms, while rest typically offers temporary relief.
When to seek further assessment
If you’re experiencing these symptoms regularly, especially if they are worsening over time, it’s important to speak with your GP. They may refer you for imaging (such as an X-ray) or to a specialist like Dr George Awwad for further evaluation. Early diagnosis can help guide the most appropriate treatment options and support your long-term joint health.
Are you a candidate for hip replacement surgery?
If you’re living with long-standing hip pain that no longer responds to non-surgical treatments, you may be considering whether hip replacement surgery could help. Total hip replacement is typically considered for individuals with advanced joint damage that affects mobility, independence, and quality of life, particularly when conservative measures are no longer effective.
Key factors that may indicate surgery is appropriate
You may be considered a suitable candidate for hip replacement if:
-
Pain is persistent and interferes with daily life
This might include difficulty walking, using stairs, getting in and out of a chair or car, or performing routine household tasks. -
Joint stiffness or limited range of motion restricts movement
Reduced flexibility can make it hard to dress, bend, or sit comfortably. -
You require walking aids for support
Needing a cane, crutches, or walker may signal significant joint deterioration. -
Imaging shows advanced joint changes
X-rays or scans may reveal cartilage loss, bone spurs (osteophytes), joint space narrowing, or deformity. -
Non-surgical treatments have not provided lasting relief
If physiotherapy, medications, weight loss, and joint injections have been trialled with little benefit, surgery may be discussed as the next step.
General health and surgical readiness
Candidacy for hip replacement is not based on age alone. What matters most is your overall health, your ability to participate in rehabilitation, and whether surgery is likely to improve your long-term mobility and comfort. Some patients with other medical conditions may require additional planning to ensure safety and optimal outcomes. Dr George Awwad will carry out a thorough assessment, taking into account your symptoms, imaging, lifestyle, and health history. If surgery is suitable, he will discuss the most appropriate timing and approach and guide you through a personalised care plan from preparation to recovery.
Who may not be suitable for hip replacement surgery?
While total hip replacement can be an effective treatment for advanced arthritis, it is not the right option for everyone at every stage. In some cases, surgery may be delayed, avoided, or reconsidered based on your symptoms, medical history, or current life circumstances. The decision to proceed with surgery involves careful consideration of risks, benefits, and overall readiness.
Reasons hip replacement may not be recommended at this time
You may not be considered suitable for hip replacement surgery if:
-
Your symptoms are still manageable
If hip pain is mild, infrequent, or doesn’t significantly interfere with daily activities, surgery may not yet be necessary. -
Imaging does not show advanced joint damage
X-rays or other scans might not reveal structural changes that would benefit from a joint replacement, even if you are experiencing discomfort. -
Non-surgical treatment is still being trialled
Options such as physiotherapy, anti-inflammatory medications, weight management, or joint injections may still offer effective symptom relief. -
There is an active infection
Any ongoing infection (skin, urinary, dental, or otherwise) increases the risk of complications and must be treated before surgery can proceed. -
Underlying health conditions increase risk
Conditions such as poorly controlled diabetes, heart or lung disease, severe obesity, or immune suppression may make surgery unsafe until better managed. -
You are not ready for recovery and rehabilitation
Hip replacement requires a commitment to post-operative rehabilitation. If you are currently unable to access support, physiotherapy, or mobility assistance, surgery may be postponed until these factors are in place.
Ongoing review and reassessment
Hip arthritis is often a progressive condition. Even if surgery is not appropriate now, your situation may change over time. Regular follow-up allows for timely reassessment of your symptoms, imaging, and overall health. If pain worsens or your function declines, Dr George Awwad will review your options and discuss whether hip replacement may be suitable at a later stage.
Anterior & posterior hip replacement surgical approaches explained
Total hip replacement surgery can be performed through different surgical approaches, depending on the patient’s anatomy, the extent of joint damage, and the surgeon’s clinical judgement. The two most common techniques are the anterior approach and the posterior approach. Dr George Awwad performs the majority of hip replacements using the anterior minimally invasive approach, based on its advantages for suitable patients.
The anterior approach involves accessing the hip joint through an incision at the front of the hip. This technique uses a natural intermuscular plane, meaning no major muscles are cut during the procedure. As a result, there may be less soft tissue trauma and a quicker return to mobility in the early stages of recovery.
Potential benefits of the anterior approach include:
- A smaller surgical incision
- Reduced disruption to muscles and soft tissues
- Earlier mobilisation after surgery
- Lower early dislocation risk in certain patients
- More consistent leg length restoration
The anterior approach is technically demanding and requires specific training, experience, and equipment. Dr Awwad has completed dedicated training in this technique and performs it in most cases where it is considered safe and appropriate for the individual.

The posterior approach: A traditional and effective option
In some situations, the posterior approach, which involves an incision at the back of the hip, may be the most appropriate option. It provides excellent visibility of the hip joint and may be preferred in patients with:
- Complex hip anatomy
- Previous surgery or scar tissue
- Certain musculoskeletal conditions requiring enhanced access
The posterior approach remains a safe and effective technique, and when performed carefully, can provide excellent long-term outcomes similar to the anterior approach.

A patient-specific decision
Dr Awwad selects the surgical approach based on your individual condition, medical history, and goals. During your consultation, he will explain the approach recommended for your surgery, outline the reasoning behind it, and answer any questions you may have. Regardless of the technique used, the goal is always the same: to restore comfort, mobility, and long-term joint function with precision and care.
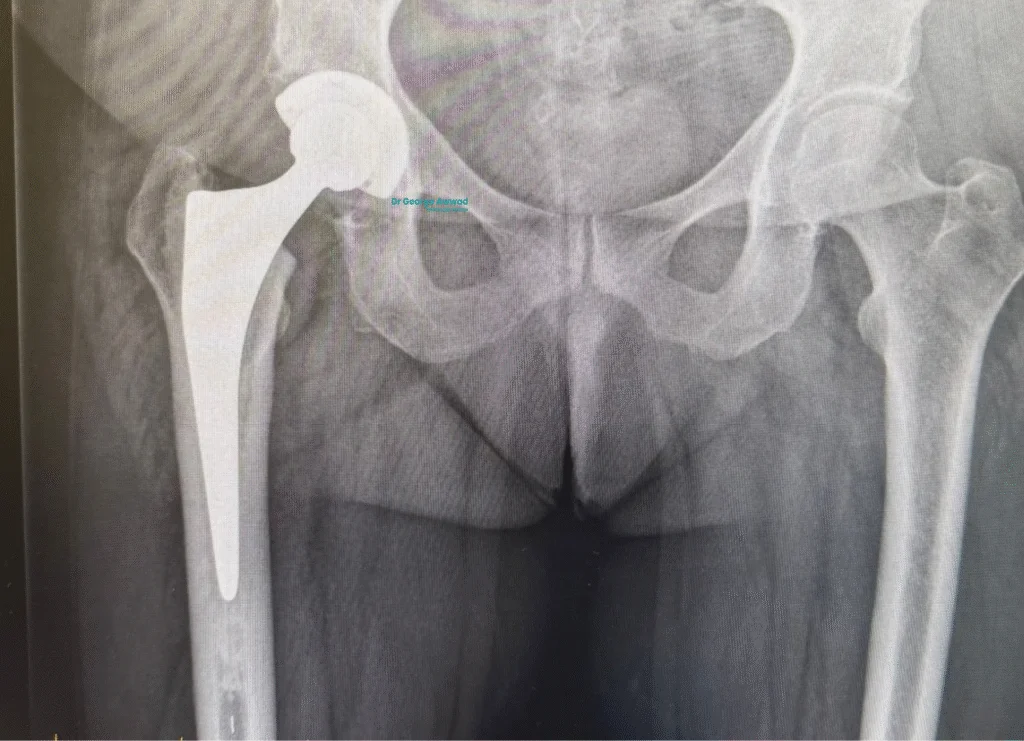
The role of imaging and surgical planning in hip replacement surgery
A well executed hip replacement begins with careful planning. Before entering the operating theatre, Dr George Awwad uses a combination of advanced imaging and digital planning tools to ensure your hip replacement is accurately tailored to your anatomy. This level of detail helps improve implant positioning, joint alignment, and long-term function.
Imaging used to assess your hip joint
The planning process typically begins with X-rays to assess joint space, bone structure, leg length, and the degree of arthritis present. In most cases, a CT scan is also arranged to provide a high resolution, three dimensional view of the hip joint and surrounding bone.
These images allow Dr Awwad to:
- Assess the shape and orientation of your hip joint
- Select the appropriate implant sizes
- Plan optimal positioning of the femoral and acetabular components
- Identify any anatomical variations that may affect the surgery
- Reduce uncertainty during the procedure
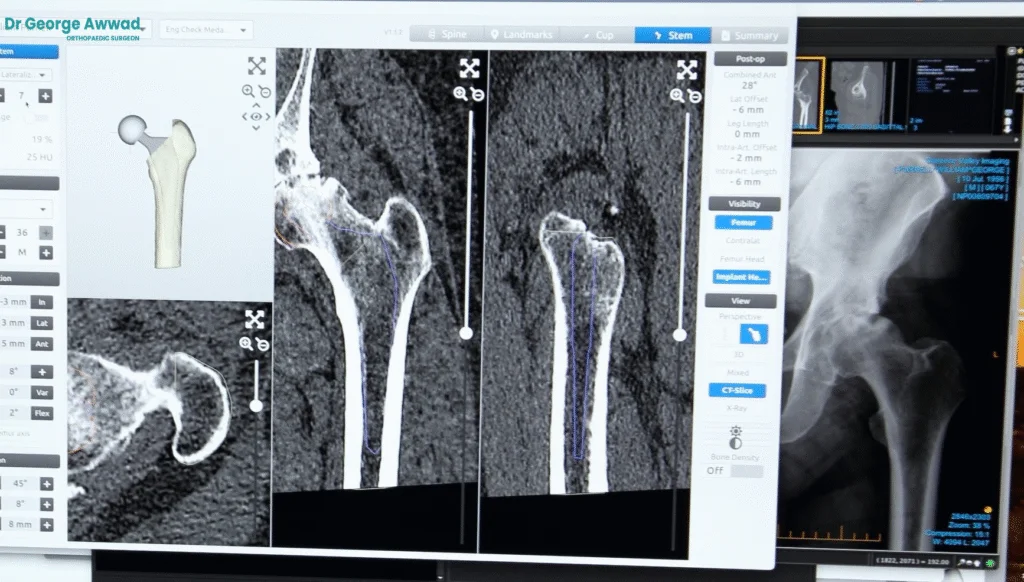
Digital 3D planning with MyHip software
Using specialised planning software (such as MyHip), Dr Awwad creates a 3D model of your hip based on the CT scan. This virtual model allows for precise pre-operative templating, helping to optimise:
- Joint alignment
- Leg length balance
- Implant fit and placement
This detailed plan is used to guide surgical decisions and supports consistent, personalised outcomes for each patient.
Patient-specific surgical tools
In select cases, Dr Awwad may also use patient-specific surgical instruments, which are created using your individual imaging data. These custom guides help accurately position the implants during surgery and are particularly useful in patients with complex anatomy or when performing revision hip replacement.

A focus on precision and safety
By combining high-quality imaging with digital planning, Dr Awwad is able to take a tailored, evidence-based approach to every procedure. This technology supports greater surgical precision, reduced variability, and improved post-operative joint function, all with the goal of helping you return to movement with confidence.
Types of hip implants used in total hip replacement
During a total hip replacement, the damaged parts of the hip joint are replaced with prosthetic components designed to restore function, reduce pain, and support long-term mobility. Dr Awwad selects each implant based on your unique anatomy, lifestyle, and long-term goals.
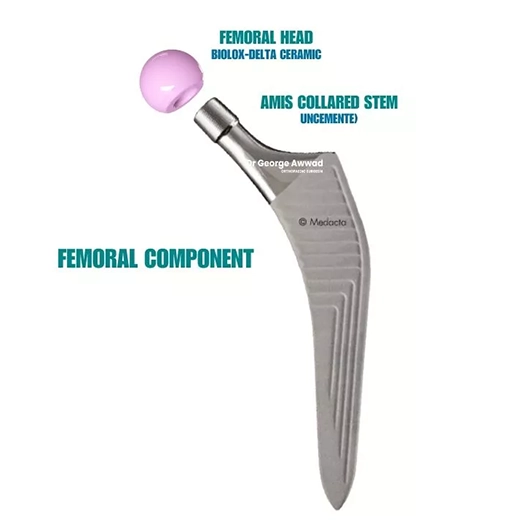

Main components of a hip replacement
A typical total hip replacement involves three key components:
- Acetabular cup – This replaces the hip socket. It is usually made of a strong metal and contains a smooth inner liner made of polyethylene or ceramic, allowing the joint to move freely.
- Femoral stem– Inserted into the thigh bone (femur), this metal component provides the foundation for the artificial joint. Stems come in various shapes and sizes to match the patient’s bone structure.
- Femoral head – The ball component fits into the socket and mimics the natural head of the femur. It may be made of ceramic or metal, depending on individual needs.
Implant fixation: Cemented vs uncemented
Dr Awwad uses either cemented, uncemented, or hybrid fixation methods based on your bone quality and health profile:
- Cemented implants are held in place with bone cement and are often used in patients with softer bone or lower bone density.
- Uncemented implants have a porous surface that encourages natural bone growth into the implant (known as osseointegration), offering a biological bond over time. These are often used in younger, active patients with good bone quality.
- Hybrid fixation uses a combination, typically a cemented femoral stem and an uncemented acetabular cup—depending on what provides the best long-term outcome.
Implant designs: Dual mobility for enhanced stability
In many cases, Dr Awwad uses a dual mobility cup, a specialised design intended to reduce the risk of dislocation and provide greater joint stability. This implant includes two points of articulation:
- An inner bearing for smooth joint movement
- An outer bearing for extended range and enhanced stability
This type of implant may be especially beneficial for patients with a higher risk of instability or those with increased activity demands.
Bearing surface combinations
The bearing surface refers to the contact point between the femoral head and the cup liner. The right combination is selected based on your age, activity level, and risk profile:mobility cup, a specialised design intended to reduce the risk of dislocation and provide greater joint stability. This implant includes two points of articulation:
- Ceramic-on-polyethylene – Common and durable, offering smooth motion and excellent long-term wear characteristics.
- Ceramic-on-ceramic – Offers high wear resistance and is often used in younger, active patients.
- Metal-on-polyethylene – May still be used in certain clinical scenarios, particularly when ceramic is not suitable.
Dr Awwad selects the most appropriate combination based on clinical evidence and individual factors to support a lasting result.
Implant system: The AMIS femoral stem
For most anterior approach hip replacements, Dr Awwad uses the AMIS femoral stem, a prosthesis designed specifically for minimally invasive surgery. This stem supports a secure fit in the femur, allows for reduced soft tissue disruption, and may assist with early mobilisation and long-term stability when used in the right patient.
Implant longevity and performance
Modern hip implants are engineered to last. While results vary, many prosthetic joints continue to perform well for 15 to 20 years or longer. Implant longevity depends on several factors:file:
- The type of implant and materials used
- Your age and activity level
- Surgical precision and joint alignment
- Ongoing care after surgery
Dr Awwad is committed to using high-quality, evidence-based implants and tailoring each component to suit your individual needs and goals.
What are the potential risks of hip replacement surgery?
While total hip replacement is generally a safe and effective procedure, as with all surgeries, there are potential risks and complications. Understanding these risks can help you make an informed decision and take proactive steps to support a smooth recovery.
Common risks of hip replacement surgery
- Infection: Infection may occur at the skin incision or around the implanted prosthesis. To reduce this risk, antibiotics are given before and after surgery, and sterile surgical protocols are carefully followed.
- Blood clots: Clots can form in the veins of the legs (deep vein thrombosis) and, more rarely, travel to the lungs (pulmonary embolism). Preventive strategies include blood-thinning medications, compression devices, and encouraging early movement after surgery.
- Dislocation of the hip joint: If the artificial ball slips out of the socket, a dislocation can occur. This risk is minimised through careful implant selection, precise surgical technique, and following post-operative precautions during early recovery.
- Leg length difference: In some cases, patients may notice a slight difference in leg length following surgery. Surgical planning aims to restore leg balance, but minor differences can sometimes occur.
- Implant wear or loosening over time: Hip replacements are designed to last many years, but over time the prosthetic components may loosen or wear, particularly with high-impact activities. If this occurs, revision surgery may be needed in the future.
- Nerve or blood vessel injury: Rarely, nearby nerves or blood vessels may be injured during surgery. These cases are uncommon and are usually temporary, but they can lead to numbness, weakness, or circulatory changes in the leg.
How risks are minimised
Dr George Awwad takes a meticulous approach to surgical planning and post-operative care. During your consultation, he will assess your individual risk factors including any medical conditions or medications that may affect healing and discuss strategies to reduce your risk of complications.
Following pre-operative instructions, attending your post-operative reviews, and participating in rehabilitation as advised can all play a key role in reducing risks and supporting your recovery.
What are the benefits of total hip replacement surgery?
For individuals living with advanced hip arthritis or joint damage, persistent pain and reduced mobility can significantly affect everyday life. When non-surgical treatments no longer provide relief, total hip replacement surgery may offer a way to restore comfort and function.
Potential benefits of hip replacement surgery
- Relief from persistent pain: Chronic hip pain is one of the most common reasons patients consider surgery. If discomfort continues despite rest, medications, or physiotherapy, hip replacement may help reduce or eliminate this pain; improving sleep, reducing reliance on walking aids, and easing daily movement.
- Improved mobility and joint function: Hip arthritis can limit your range of motion, making it difficult to bend, dress, or get in and out of a car. Following recovery, many patients report increased flexibility, improved walking ability, and a return to daily tasks with less effort and discomfort.
- Enhanced independence and quality of life: Severe hip pain can affect your ability to work, exercise, or participate in social and recreational activities. By replacing the damaged joint with a well-aligned prosthesis, hip replacement may support greater independence, enabling you to walk more comfortably, travel with ease, and enjoy everyday activities again.
Managing expectations
While most patients experience meaningful improvement in pain and function, outcomes can vary depending on factors such as age, overall health, and the degree of joint damage. The goal of surgery is to improve mobility and reduce pain, not necessarily to return to high-impact sports or intense physical activity.
During your consultation, Dr Awwad will provide clear guidance on what you can expect based on your individual condition, and how to prepare for the best possible outcome.
Your hip replacement journey with Dr George Awaad
Choosing to undergo total hip replacement is a major decision. Dr George Awwad is committed to guiding you through the process with clear communication, careful planning, and individualised care. From your initial consultation to your recovery at home, every stage is designed to support your safety, comfort, and confidence.
1. Initial consultation and assessment
Your journey begins with a comprehensive consultation at one of Dr Awwad’s clinics in Adelaide. During this visit:
- Your symptoms, lifestyle, activity level, and goals are discussed in detail
- A physical examination is performed to assess joint mobility, leg alignment, and walking pattern
- X-rays or a referral for advanced imaging (such as a CT scan) may be arranged
If surgery is appropriate, Dr Awwad will explain the benefits, risks, and timing, and provide guidance on how to prepare for the next steps.
2. Imaging and surgical planning
Pre-operative planning plays a critical role in the accuracy and success of your surgery:
- X-rays assess joint space and alignment
- A CT scan is used to build a detailed 3D model of your hip
- MyHip digital planning software helps determine the best implant size, alignment, and positioning
This technology allows Dr Awwad to tailor the surgery to your anatomy before entering the operating theatre.
3. Preparing for surgery
In the lead-up to your procedure, you may be asked to:
- Begin simple exercises to strengthen surrounding muscles
- Adjust or pause certain medications (in consultation with your GP or specialist)
- Attend a pre-anaesthetic assessment
- Use antiseptic washes and complete screening tests as required
You’ll also receive instructions on planning for your recovery, including organising transport home, preparing a safe recovery space, and arranging help during the early stages.
4. The day of surgery and hospital admission
Most patients are admitted to hospital on the morning of surgery. You’ll receive specific fasting and fluid instructions from the anaesthetist before admission.
Bring along:
- Admission paperwork
- Recent imaging and a list of medications
- Comfortable clothing, supportive shoes, and personal toiletries
- Any mobility aids you currently use
The hospital team will assist you through check-in and preparation for surgery.
5. The surgical procedure
Dr Awwad performs most hip replacements using the anterior minimally invasive approach (AMIS) but may use the posterior approach if clinically appropriate.
Key steps include:
- Anaesthesia – You’ll receive a spinal anaesthetic with light sedation or a general anaesthetic, based on your needs
- Surgical access – A small incision is made at the front (or back) of the hip depending on the chosen approach
- Joint preparation – The damaged femoral head is removed, and the hip socket is reshaped
- Implant insertion – The acetabular cup (often a dual mobility design) and femoral stem (such as the AMIS stem) are inserted
- Final checks – Leg length, joint alignment, and implant stability are confirmed
- Closure – The wound is closed with dissolvable sutures and a dressing is applied
You are then transferred to recovery where your vital signs and comfort are closely monitored.
6. Hospital stay and early mobilisation
Most patients stay in hospital for 2 to 4 days. During this time:
- Physiotherapists will assist you to begin walking, often within 24 hours
- Pain management, wound care, and mobility strategies are provided
- Discharge planning ensures you are safe and supported at home
7. Recovery at home and follow-up care
Your rehabilitation continues after you return home and typically includes:
- Ongoing physiotherapy and home exercises
- A gradual return to walking and daily activities
- Review appointments with Dr Awwad to monitor your progress
Follow-up schedule:
- Day 10 – Wound review
- 6–8 weeks – Post-operative assessment
- 12 months – Annual review and longer-term follow-up if required
This personalised care ensures your recovery stays on track and any concerns are addressed promptly.
Pain management after hip replacement
Effective pain control is an important part of your recovery after total hip replacement. Well-managed pain can help you move more comfortably, sleep better, and fully engage in physiotherapy, all of which support faster healing and reduce the risk of complications.
Dr George Awwad and the hospital team use a multimodal approach to pain relief, combining different strategies to manage discomfort from multiple sources while minimising side effects.
How pain is managed after surgery
Pain control begins in the operating theatre and continues throughout your hospital stay and return home. Techniques may include:
- Spinal or nerve block anaesthesia to numb the area around the hip
- Local anaesthetic placed into the joint during surgery to ease early pain
- Anti-inflammatory medications to reduce swelling
- Paracetamol for baseline pain management
- Opioid medications, used in low doses and only when necessary
- Ice therapy to reduce local swelling and discomfort
- Guided movement to prevent stiffness and support circulation
Immediately after surgery
In the recovery room, your pain will be closely monitored. Some discomfort around the incision and hip is expected, but the goal is to keep pain well controlled. You may have:
- A nerve catheter or spinal block that provides temporary numbness
- Scheduled oral medications to maintain comfort
- Access to additional pain relief if needed
You’ll be supported to begin gentle movement soon after surgery, as early mobility plays a key role in reducing stiffness and enhancing recovery.
Pain management during your hospital stay
Once the effects of spinal or nerve block wear off, oral pain medications become the primary method of control. These will be:
- Given at regular intervals to prevent pain build-up
- Adjusted based on your response or any side effects
- Supported by breakthrough medication for additional relief if required
Physiotherapy will begin during this time, and your pain relief plan will be designed to support comfortable participation in movement and walking.
Pain relief at home
After discharge, you’ll receive a personalised pain management plan, which may include:
- A clear medication schedule
- Guidance on reducing stronger medications over time
- Recommendations for ice therapy and pacing your activity
- Advice on when to contact the clinic if pain increases unexpectedly
Most patients are able to stop using strong pain medication within 1 to 2 weeks, continuing with paracetamol or anti-inflammatories as needed.
What to expect during recovery
It’s normal to experience some discomfort in the early recovery phase. You may notice:
- General soreness in the hip, thigh, or buttock
- A tight or pulling sensation during movement
- Mild stiffness after rest
- A low-level ache that eases with activity
These symptoms typically improve over the first few weeks and continue to settle as your joint heals.
Monitoring and long-term improvement
Pain should gradually reduce over time. Most patients report significant improvement in discomfort within 4 to 6 weeks, with ongoing gains in comfort and function in the months that follow. If you experience increasing pain, signs of infection, or anything unusual, Dr Awwad’s team is available to provide prompt support.
Follow-up appointments allow your pain relief plan to be reviewed and adjusted as needed, ensuring your recovery remains on track.
Hip replacement recovery timelines: what to expect
Recovery after total hip replacement is a gradual process, and healing timelines vary between individuals. Your progress will depend on factors such as age, general health, activity level, and the complexity of your surgery. Dr George Awwad will guide you through each stage of your recovery and tailor your plan to match your individual needs.
In hospital (Day 0 to Day 2–4)
- You will usually begin standing and walking (with assistance) on the same day or the day after your surgery.
- Physiotherapists will help you move safely using a walking frame or crutches.
- Your wound will be monitored and kept covered with dressings.
- Pain is managed with a combination of oral and injectable medications.
Before discharge, you must be able to:
- Walk safely using mobility aids
- Navigate stairs (if needed at home)
- Understand wound care and your home exercise program
Week 1 to Week 3
- You will continue using crutches or a walker for support at home.
- Daily physiotherapy exercises are important to restore movement, strength, and confidence.
- Swelling, bruising, stiffness, and fatigue are common and expected during this phase.
Week 4 to Week 6
- Many patients begin transitioning from walking aids to unaided walking, depending on balance and comfort.
- You may resume light daily activities, such as short outdoor walks or gentle household tasks.
- A follow-up appointment with Dr Awwad will assess wound healing, joint alignment, and early progress.
- Driving may be resumed if you have stopped strong pain medication and feel safe using your operated leg. Always check with your surgeon and car insurer before returning to driving.
Week 6 to Week 12
- Most patients walk independently with improved joint stability and reduced pain.
- Physiotherapy may progress to include strength, balance, and endurance exercises.
- Many patients return to part-time or full-time work, depending on the physical demands of their role.
- Sexual activity is usually safe after 6 to 8 weeks, as long as you feel comfortable. Avoid positions that strain the hip or increase the risk of dislocation. Speak with your GP if you’re unsure.
Month 3 to Month 12
- You should notice ongoing improvements in strength, flexibility, and confidence with movement.
- Many patients return to low-impact activities like swimming, cycling, yoga, and walking on uneven surfaces.
- By this stage, significant reductions in pain and improved function are expected.
- A 12-month review with Dr Awwad is usually scheduled to evaluate your long-term outcome.
Long-term considerations
- Your new hip is designed to reduce pain and restore mobility for many years.
- Avoid high-impact sports or twisting movements unless advised otherwise.
- Staying active, maintaining a healthy weight, and continuing regular exercise can help protect your implant.
- If you notice increased pain, swelling, stiffness, or signs of infection (such as redness, fever, or discharge), seek medical attention promptly.
Precautions to follow during your hip replacement recovery
Recovering safely after hip replacement surgery is essential for protecting your new joint and achieving the best possible outcome. In the first few weeks after surgery, being careful with your movements, taking your medications as directed, and following your physiotherapy plan can reduce the risk of complications and support your long-term recovery.
Wound care
- Your surgical wound will be covered with a waterproof dressing so you can shower while keeping the area clean and protected.
- Avoid soaking the wound in baths or swimming pools until it has fully healed.
- Most incisions are closed with dissolvable stitches that do not require removal.
- Contact your GP if you notice any signs of infection, such as redness, warmth, increasing swelling, fluid leakage, or fever.
Medication and pain control
- You will be prescribed medications to help manage pain, reduce inflammation, and prevent blood clots.
- Follow the medication schedule provided at hospital discharge and report any side effects or concerns.
- Pain and swelling will gradually improve, although some discomfort is common for several weeks after surgery.

Mobility and weight-bearing
- Most patients begin walking with a physiotherapist within 24 hours of surgery.
- Depending on the surgical approach used and your individual case, you may be allowed to fully bear weight immediately or increase it gradually.
- Your physiotherapist will guide you through safe walking techniques, stair navigation, and exercises to rebuild strength and confidence.
Movement precautions
The precautions you need to follow depend on whether your surgery was performed using the anterior (front) or posterior (back) approach. These guidelines help protect the joint while the surrounding muscles and soft tissues heal.
If you had an ANTERIOR APPROACH (AMIS):
This method typically allows for quicker mobilisation and has fewer movement restrictions, however:
- Avoid extending your leg too far behind you / keep your hip in a neutral position.
- Try not to overstride or push your leg backward when standing or walking.
- This restriction usually applies for the first 6 weeks.
If you had a POSTERIOR APPROACH:
This method requires more specific precautions to help prevent dislocation:
- No twisting at the hips - keep your feet, knees, and hips aligned. Turn your entire body instead of twisting at the waist.
- Avoid bending beyond 90 degrees - do not bend forward to pick things up from the floor or sit in very low chairs.
- Do not cross your legs or ankles - maintain a neutral hip position when sitting or lying down.
Dr Awwad or the physiotherapist will advise you when it is safe to relax these precautions, typically after 6 weeks.
Sleeping and resting positions
- Sleep on your back or on your non-operative side with a pillow placed between your knees.
- Avoid sleeping on your stomach or turning your leg inward during rest.
- Take care when getting in and out of bed to avoid putting stress on your hip.
Avoiding falls and injury
- A fall in the early recovery phase can be serious. Use your mobility aids until advised otherwise.
- Create a safe environment at home by:
- Removing loose rugs or trip hazards
- Using non-slip mats in wet areas
- Installing grab rails in the bathroom if needed
- Wearing well-fitted, non-slip shoes indoors
Returning to daily activities
- You can usually resume light household activities within a few weeks, depending on your recovery progress.
- Avoid bending deeply, lifting heavy objects, or making sudden twisting movements until you have been cleared by Dr Awwad.
- Driving may resume when you are no longer taking strong pain medication and can safely control your vehicle, usually between 4 to 6 weeks post-op. Always check with Dr Awwad and even your insurer before returning to driving.
Physiotherapy after hip replacement surgery
Physiotherapy is an essential part of your recovery following total hip replacement. A structured rehabilitation program helps restore strength, balance, and flexibility so you can safely return to your daily activities. Your physiotherapy journey begins within the first 24 hours after surgery and continues for several weeks or months as you progress.
Early physiotherapy in hospital
Soon after surgery, your physiotherapist will help you begin gentle exercises. Early movement is important to:
- Prevent stiffness and blood clots
- Rebuild muscle memory
- Support circulation and joint mobility
Initial exercises may include:
- Ankle pumps and foot circles, to keep blood flowing
- Leg slides and gentle stretches, to improve mobility
- Standing and short walks, with the support of a frame or crutches
The focus is on helping you regain confidence and mobility while protecting your new joint.
Rehabilitation after discharge
Once you return home or to a rehabilitation centre, your physiotherapy program becomes more targeted and intensive. It will be tailored to your condition, goals, and progress.
You may work on:
- Strengthening the muscles around your hip, thigh, and core
- Improving flexibility with stretching and range-of-motion exercises
- Gait retraining to help you walk more evenly and confidently
- Balance and coordination activities to reduce the risk of falls
Your physiotherapist will monitor your progress and adjust your program as needed to suit your comfort and goals.
Benefits of physiotherapy after hip replacement
Ongoing physiotherapy can:
- Reduce post-operative swelling and joint stiffness
- Improve your walking pattern and movement control
- Support muscle strength and joint stability
- Lower the risk of complications like blood clots or joint dislocation
- Help you safely return to work, driving, or low-impact exercise
Staying committed to your recovery
Your success depends on your active participation. Consistency is key:
- Perform your exercises daily between physiotherapy sessions
- Follow your therapist’s advice closely, especially on movement techniques
- Don’t push through pain, let your physiotherapist know if something feels uncomfortable
Even once your formal rehab ends, continuing a regular exercise routine can help protect your joint and maintain your mobility in the long term.
Returning to activity after hip replacement surgery
A key goal of total hip replacement is to help you return to a more active and comfortable life. As you recover, you may find that everyday tasks become easier and that you are able to enjoy more of the activities you once loved. While it is important to protect your new joint during the healing period, many patients are able to resume a wide range of hobbies and routines with the right support and guidance.
Activities you can expect to return to
With time and recovery, you may gradually return to:
- Walking without a limp or pain
- Climbing stairs more comfortably
- Gardening, playing with children or grandchildren, and light housework
- Recreational activities such as swimming, golf, or cycling
- Work duties, depending on your occupation
- Social outings and community involvement
The timeline will vary based on your general health, the physical demands of each activity, and how your recovery progresses.
Activities that may need to be modified
Some high-impact or contact sports may not be recommended after hip replacement because of the increased risk of wear or dislocation. These may include:
- Running or jogging on hard surfaces
- Sports that involve sudden twisting, jumping, or collisions (such as football or basketball)
- Heavy lifting or repetitive bending
If you are unsure whether a certain activity is safe, speak with your GP, physiotherapist or call Dr Awaad’s room for individualised advice.
Safe movement habits to protect your new hip
As you resume daily activities, you may be given strategies to reduce stress on the joint, such as:
- Using supportive footwear to avoid slips or imbalance
- Avoiding low chairs or deep squatting during the early stages of recovery
- Practising correct bending and lifting techniques
- Maintaining a healthy weight to reduce joint strain
These habits can help preserve your hip replacement and support long-term function.
Staying active for long-term joint health
Ongoing movement is vital. Low-impact exercise not only helps to strengthen muscles and maintain joint mobility but also supports your cardiovascular health and overall wellbeing. Many people find that they are more confident, active, and independent after surgery than they were before.
You will be guided through this transition with regular follow-up and support to make sure your return to activity is safe and sustainable.
Hip replacement surgery FAQ’s
How long does total hip replacement surgery take?
The procedure generally takes about 60 to 90 minutes. Additional time may be required for preparation, anaesthesia, and post-operative monitoring. Most patients spend 2 to 4 days in hospital after surgery, depending on your recovery and overall health.
How long will my hip replacement last?
Most modern hip implants are designed to last 15 to 25 years or more, especially when looked after properly. Factors like your activity level, weight, and general health can all influence the lifespan of your implant. Dr Awwad will discuss the most suitable implant for your situation during your consultation.
What type of implant is used in a hip replacement?
Hip replacements typically involve three main components:
- Acetabular cup (socket)
- Femoral stem
- Femoral head
Dr Awwad selects implants made from durable materials such as ceramic, polyethylene, or metal, based on your age, anatomy, bone quality, and lifestyle.
What are the risks or complications of hip replacement?
Although most patients recover well, potential complications include:
- Infection
- Blood clots
- Dislocation
- Nerve or blood vessel injury
- Leg length discrepancy
- Implant loosening or wear over time
Dr Awwad will explain all potential risks and steps taken to reduce them during your consultation and surgical planning.
How do I prepare for hip replacement surgery?
Preparation includes:
- Completing any pre-operative tests
- Attending a pre-admission clinic
- Reviewing your medications
- Getting your home ready (e.g. removing trip hazards, arranging mobility aids)
Maintaining a healthy weight and strengthening surrounding muscles may help improve your recovery. Dr Awwad and his team will guide you through every step.
What is the recovery like after surgery?
You will begin walking, usually with a frame or crutches, within 24 hours after surgery. Physiotherapy starts early and continues after discharge. Most patients return to routine activities within 6 to 12 weeks, with ongoing improvements up to 12 months. Everyone’s recovery is different and tailored advice will be provided based on your progress.
When can I return to work or hobbies?
This depends on your job and activity level:
- Desk-based work: 4–6 weeks
- Physical jobs: 10–12 weeks or more
- Low-impact hobbies (like swimming or cycling): often resumed after 6–8 weeks
- High-impact sports (like running or football): may need to be avoided or modified long term
Dr Awwad will provide specific recommendations based on your goals.
Can I drive after surgery?
Most patients return to driving around 4–6 weeks after surgery, once they are no longer taking strong pain medication and can confidently move their leg and operate pedals. Always check with Dr Awwad before resuming driving.
Are there different surgical approaches? Does it affect recovery?
Yes. Dr Awwad uses a surgical approach based on your anatomy and surgical needs. Common approaches include:
- Anterior approach (from the front)
- Posterior approach (from the back)
Each approach has benefits, and there is no proven long-term advantage of one over another. The key factor is that your surgery is well-planned and performed safely.
What should I avoid after hip replacement surgery?
To protect your new hip in the early recovery phase, you may be advised to:
- Avoid deep bending or twisting
- Refrain from high-impact activities
- Use supportive footwear
- Maintain a healthy weight
Your physiotherapist will provide specific precautions to follow.
How will I know if my hip replacement is healing properly?
You will have regular follow-up appointments with Dr Awwad to monitor your recovery, check your wound, assess your mobility, and take post-operative imaging if required. If you experience increasing pain, swelling, or other concerning symptoms, you should contact Dr Awwad’s rooms promptly.
