ACL Reconstruction and Knee Ligament Treatment
Treatment options for ACL injuries and other ligament damage to the knee
The ligaments in your knee play a critical role in maintaining joint stability, especially during activities that involve twisting, pivoting, or rapid changes in direction. Injuries to these ligaments, particularly the anterior cruciate ligament (ACL), are common in sports and high impact activities, but can also occur due to falls, accidents, or sudden trauma.
ACL tears and other ligament injuries often lead to pain, swelling, a sense of instability, and limitations in physical function. In some cases, non-surgical management such as physiotherapy may be appropriate. In others, especially where the knee is unstable or the patient is highly active, surgical treatment may be recommended to restore function and support long term joint health.
This page explores the role of knee ligaments, common causes of injury, and the surgical treatment options available, including ACL reconstruction and procedures for other ligament injuries such as MPFL (medial patellofemoral ligament) repair, PCL reconstruction, and multi-ligament knee reconstruction. You’ll also learn what to expect before, during, and after surgery, and how rehabilitation plays a key role in recovery.
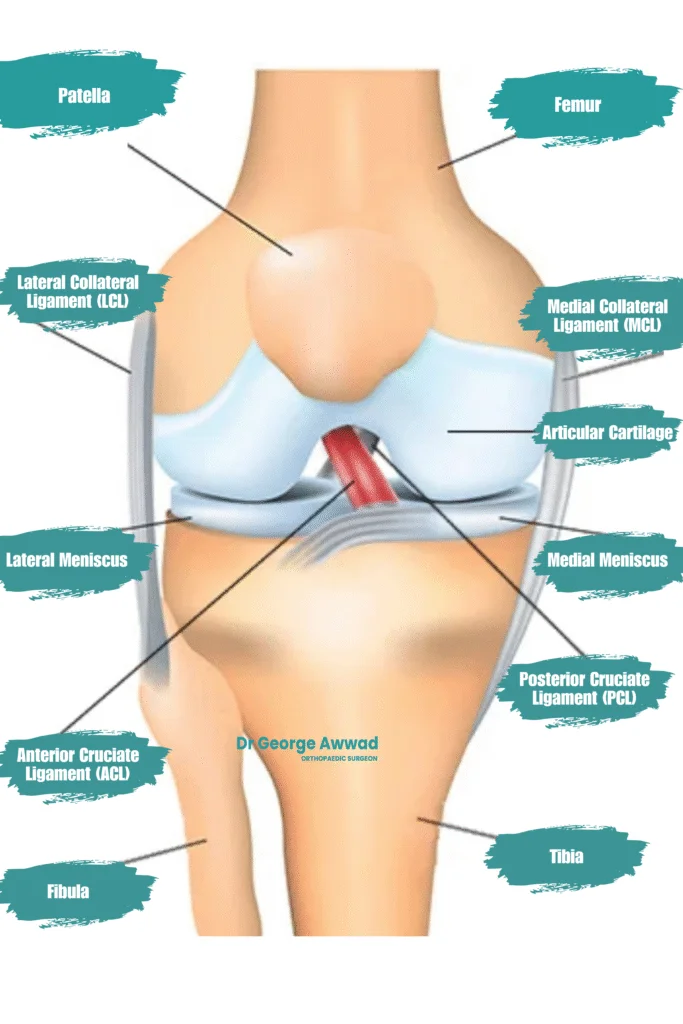
Understanding knee ligaments and how injuries occur
Key ligaments in the knee
- Anterior Cruciate Ligament (ACL): One of the most commonly injured ligaments, the ACL runs diagonally through the centre of the knee and helps control rotational stability as well as forward movement of the tibia (shinbone) on the femur (thighbone).
- Posterior Cruciate Ligament (PCL): Located behind the ACL, the PCL prevents the tibia from moving too far backwards.
- Medial Collateral Ligament (MCL): Found on the inner side of the knee, the MCL stabilises against inward forces that push the knee sideways.
- Lateral Collateral Ligament (LCL): Positioned on the outer side of the knee, the LCL resists forces that push the knee outward.
- Medial Patellofemoral Ligament (MPFL): This ligament helps stabilise the patella (kneecap), particularly during movement or impact.
How knee ligament injuries occur
- Sudden stops or changes in direction: Especially in sports such as soccer, netball, basketball, or skiing.
- Direct trauma: A blow to the outside or front of the knee (e.g. in a tackle or fall).
- Landing awkwardly: From a jump or uneven surface, particularly with the knee in a rotated or extended position.
- Hyperextension or over-straightening of the knee: Which may stretch or tear the ACL or PCL.
- Grade 1: Mild sprain with slight stretching of the ligament.
- Grade 2: Partial tear, often causing some looseness or instability.
- Grade 3: Complete tear or rupture, leading to significant instability and potential joint dysfunction.
How ligament injuries are diagnosed
Initial assessment and medical history
- Whether the knee twisted, hyperextended, or experienced a direct blow
- Any sensation of a “pop” or “snap” at the time of injury
- Immediate swelling or instability after the event
- Difficulties with walking, weight-bearing, or knee movements
Physical examination
Dr Awwad will carefully assess your knee using specific clinical tests to evaluate the stability of each ligament. These may include:
- Lachman test or anterior drawer test – to assess the anterior cruciate ligament (ACL)
- Pivot shift test – to detect ACL deficiency and rotational instability
- Posterior drawer test – to assess the posterior cruciate ligament (PCL)
- Valgus and varus stress tests – to assess the medial (MCL) and lateral (LCL) collateral ligaments
- Joint line tenderness or locking – may suggest associated meniscal injury
Imaging tests
- X-rays: Although ligaments are not visible on X-ray, this imaging helps detect fractures, bone avulsion injuries, or signs of joint misalignment.
- MRI (Magnetic Resonance Imaging): This is the gold-standard for visualising soft tissues inside the knee. MRI can confirm complete or partial ligament tears, assess meniscal damage, and provide a detailed view of the cartilage, joint capsule, and surrounding soft tissues.
- Ultrasound: Occasionally used to evaluate superficial structures like the MCL, although it is not routinely used for deeper ligaments such as the ACL.
- Stress radiographs: In some complex or chronic cases, these may be used to evaluate instability under controlled stress.
When immediate diagnosis is not possible
Surgical treatment options for ACL and other ligament injuries
ACL Reconstruction
- The torn ACL is replaced with a graft, usually taken from the patient’s own hamstring or patellar tendon.
- A tunnel is drilled into the femur and tibia to position the new ligament in the same orientation as the original ACL.
- The graft is fixed securely, and over time, it integrates into the bone to function as a new ligament.
PCL, MCL, and LCL Reconstruction or Repair
- PCL reconstruction: Similar to ACL surgery, a graft is used to replace the damaged ligament. This may be performed in combination with ACL surgery if both are injured.
- MCL/LCL repair or reconstruction: May involve direct repair of torn ligaments or graft reconstruction depending on the injury location and chronicity.
Multi-Ligament Knee Reconstruction
- Comprehensive pre-operative imaging and planning
- Reconstruction of two or more ligaments (e.g. ACL + PCL, or ACL + MCL + LCL)
- Careful coordination of surgical timing and rehabilitation phases
ACL reconstruction surgery: techniques and graft types
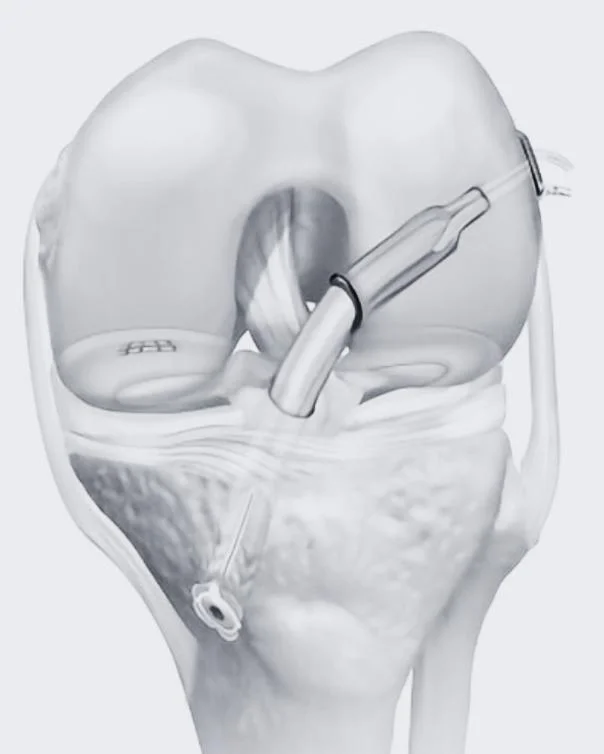
Key surgical techniques
Dr Awwad uses arthroscopic (keyhole) techniques for ACL reconstruction, which means the surgery is performed through small incisions with the help of a camera and specialised instruments. This minimally invasive approach allows for:
- Less soft tissue trauma
- Reduced post-operative pain
- Lower risk of infection
- Faster recovery compared to traditional open surgery
- You are in generally good health and able to participate in a structured recovery and rehabilitation program
Tunnel placement is a critical part of the procedure. Precise tunnels are created in the femur and tibia to position the graft in the same anatomical orientation as the original ACL. Accurate tunnel alignment supports graft healing and helps restore natural knee biomechanics.
Graft types used in ACL reconstruction
1. Hamstring tendon autograft
- The most commonly used graft
- Harvested from the semitendinosus (and sometimes gracilis) tendons
- Benefits: smaller incision, less anterior knee pain
- Considerations: slightly longer time to regain hamstring strength
Patellar tendon autograft
- A central third of the patellar tendon is taken, along with bone plugs from the kneecap and shinbone
- Often recommended for young athletes or those returning to high-demand sports
- Benefits: strong initial fixation, bone-to-bone healing
- Considerations: increased risk of anterior knee pain or kneeling discomfort
3. Quadriceps tendon autograft
- A robust option increasingly used in both primary and revision surgeries
- Harvested with or without a bone plug from the kneecap
- Benefits: larger graft size, less risk of anterior knee pain
- Considerations: slightly longer recovery of quadriceps strength
4. Allograft (donor tissue)
- Sterile tendon tissue sourced from a tissue donor
- May be considered in revision surgery or for patients not suitable for autograft harvest
- Benefits: avoids additional surgical site
- Considerations: longer integration time, not typically recommended for young or high-level athletes due to higher re-tear rates
Fixation and graft integration
The graft is fixed securely into the bone tunnels using screws or other fixation devices. Over the next few months, the graft undergoes biological incorporation, where it gradually becomes part of the knee’s natural structure. This process is supported by careful rehabilitation and load management during recovery.
Revision ACL surgery
- Careful pre-operative imaging (MRI and CT)
- Assessment of tunnel position and hardware from the initial surgery
- Consideration of different graft options and surgical staging if necessary
Recovery and rehabilitation after ACL surgery
Recovery following ACL reconstruction is a structured, multi-phase process designed to protect your graft, restore knee function, and gradually return you to your regular activities or sports. Dr George Awwad and his team will guide you through each stage, tailoring your care to your individual surgery, physical progress, and personal goals.
Immediately After Surgery
- Hospital stay: Most patients stay one night in hospital following surgery.
- Bracing and support: A knee brace may be used in certain cases, depending on the procedure and any associated injuries.
- Compression stockings: White stockings are used to help reduce the risk of blood clots and are typically worn for 24–48 hours. You can stop wearing them once you're regularly mobile. If you develop calf pain, swelling, or redness, contact Dr Awwad’s office or the hospital immediately
- Wound care: The bulky outer dressing is usually removed the day after surgery. Smaller adhesive dressings over your incision should remain intact until reviewed. Bagging the knee in plastic while showering is advised. A wound check is typically scheduled 1–2 weeks post-operatively
- Ice and elevation: Elevate your leg and apply ice packs regularly for the first 72 hours (20–30 mins per hour) to reduce pain and swelling. Ice use can continue beyond this if it helps your comfort
Pain Management
Pain medications are tailored by your anaesthetist and may include paracetamol and short-term opioids such as Endone or Palexia. Anti-inflammatory medications are not routinely used unless advised by Dr Awwad
Rehabilitation Phases
Your physiotherapy program will begin shortly after surgery and typically continues for 12 months. Recovery is broken into five distinct phases:
Phase I (0–6 weeks): Protect and Mobilise
- Protect the graft and fixation
- Control swelling and inflammation
- Achieve full knee extension and near-normal flexion
- Restore normal walking pattern
- Patellar and scar mobilisation
- Heel slides, quadriceps isometric contractions
- Early proprioception exercises (e.g. balance work)
- Stationary cycling and hydrotherapy if available
Phase II (6–12 weeks): Build Strength and Range
Goals:
- Restore normal gait, including stair climbing
- Improve strength in the hip, thigh, and calf muscles
- Increase proprioception and flexibility
- Closed kinetic chain exercises (e.g. wall sits, lunges)
- Cycling, elliptical, and Stairmaster as tolerated
- If available, running on underwater treadmill can begin from week 8
Phase III (12–26 weeks): Advance Strength and Function
- Improve endurance and strength to prepare for sports
- Maintain joint protection
- Begin land-based running and agility preparation
- Progress to jogging around 12 weeks
- Knee extensions, strength training
- Cardiovascular training and proprioception work
Phase IV (6–9 months): Return to Agility and Sport Readiness
Goals:
- Symmetrical strength and agility performance
- Readiness for single- and triple-hop tests
- Begin sport-specific drills
- Jumping, cutting, acceleration drills
- Agility ladders, shuttle runs, sport simulations
Phase V (9–12+ months): Full Return to Sport
Goals:
- Safe and confident return to full activity or sports
- Maintain strength, endurance, and injury prevention
- Final clearance from Dr Awwad before resuming unrestricted sport
- Minimal strength deficit (<10%) compared to the other leg
- Completion of hop tests (>90% of the uninjured side)
- Completion of sport-specific rehab and running drills
When to Seek Medical Attention
Please contact Dr Awwad’s office or your hospital immediately if you experience:
- High temperatures or fevers
- Increasing redness or warmth around the incision
- Worsening pain in the calf, knee, or thigh
- Excessive bleeding or fluid discharge from the wound
PCL, MCL, and LCL Reconstruction or Repair surgical techniques
While ACL injuries are among the most well-known ligament injuries in the knee, damage to the posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) can also result in pain, instability, and functional limitation. In some cases, these injuries require surgical reconstruction or repair. Dr George Awwad provides comprehensive assessment and advanced surgical treatment for complex ligament injuries, including isolated or combined ligament reconstructions.
Posterior cruciate ligament (PCL) reconstruction
- When the PCL injury is graded as severe (Grade 3) in certain patients
- When there is combined ligament injury (e.g. ACL + PCL)
- When conservative treatment fails to restore stability
- In active individuals with ongoing instability or functional impairment
- Graft options: Typically uses autografts (such as hamstring tendons) or allografts (donor tissue)
- Tunnel placement: Bone tunnels are created in the femur and tibia to anchor the graft
- Fluoroscopic guidance: Intraoperative imaging may be used to optimise tunnel placement
- Fixation: Grafts are fixed with interference screws or buttons for secure attachment
- Rehabilitation: Requires a slower rehabilitation protocol than ACL reconstruction due to higher graft stress
Medial collateral ligament (MCL) repair or reconstruction
- Grade 3 injuries with persistent valgus instability
- Multi-ligament injuries (e.g. ACL + MCL)
- Chronic MCL laxity that fails to respond to non-operative care
- Avulsion injuries where the ligament pulls away from the bone
- Repair: In acute injuries, the ligament may be reattached to bone using suture anchors or screws
- Reconstruction: In chronic or complex cases, tendon grafts are used to reconstruct the ligament
- Anatomical reconstruction: Reproduces the native MCL path using precise tunnel placement and tensioning
- Protection and bracing: Post-operatively, a hinged knee brace is typically used for 6 weeks
Lateral collateral ligament (LCL) reconstruction
- Severe LCL tears with instability
- Combined posterolateral corner injuries
- Chronic LCL insufficiency following previous trauma
- High-demand athletes or physically active individuals with lateral knee laxity
- Graft reconstruction: Often involves use of autograft or allograft tissue
- Anatomic restoration: The graft is placed along the natural path of the LCL to restore normal biomechanics
- Posterolateral corner reconstruction: May be performed if additional structures (e.g. popliteus tendon) are involved
- Rehabilitation: Includes a protective period in a brace with a graduated return to weight-bearing and strengthening exercises
Multi-ligament reconstruction
Surgical planning with imaging and graft choice
Prior to surgery, Dr Awwad will review advanced imaging (MRI, CT scans) to assess the extent of ligament damage and joint alignment. Graft type (autograft vs. allograft) is selected based on factors such as the number of ligaments requiring reconstruction, graft availability, patient activity level, and previous surgeries.
This comprehensive approach to PCL, MCL, and LCL reconstruction aims to restore knee stability, protect surrounding joint structures, and support a safe return to activity. Dr George Awwad tailors each surgical plan to the patient’s specific injury pattern, anatomy, and functional goals.

Recovery and rehabilitation after multiligament knee surgery
Rehabilitation following multiligament knee reconstruction or repair is a structured and progressive process. It plays a crucial role in restoring knee function, protecting the surgical repairs, and reducing the risk of re-injury. Dr George Awwad follows detailed post-operative rehabilitation protocols that are tailored to the specific ligaments repaired (e.g. ACL, PCL, MCL, LCL) and individual patient factors.
Risks and potential complications of knee ligament surgery
1. Infection
2. Blood Clots (Deep Vein Thrombosis - DVT)
3. Knee Stiffness or Loss of Motion
Some patients may experience restricted movement following ligament surgery, especially if post-operative physiotherapy is delayed or inconsistent. Adhering to the prescribed rehabilitation protocol and attending regular physiotherapy sessions can help maintain and gradually restore knee motion.
4. Graft Failure or Stretching
4. Graft Failure or Stretching
In ACL or multiligament reconstructions, the graft used to reconstruct the ligament can stretch or fail, particularly in the early phases of recovery or in the setting of a new injury. This may result in persistent instability and require further surgery. Dr Awwad provides detailed guidance on activity restrictions to protect the repair during healing.
4. Graft Failure or Stretching
In ACL or multiligament reconstructions, the graft used to reconstruct the ligament can stretch or fail, particularly in the early phases of recovery or in the setting of a new injury. This may result in persistent instability and require further surgery. Dr Awwad provides detailed guidance on activity restrictions to protect the repair during healing.
5. Nerve or Blood Vessel Injury
6. Residual or Recurrent Instability
7. Graft Site Discomfort or Weakness
8. Arthrofibrosis (Scar Tissue Formation)
9. Kneecap Pain (Anterior Knee Pain)
10. Hardware Complications
Minimising Your Risk
ACL and ligament surgery FAQs
What is the difference between a ligament repair and a ligament reconstruction?
A ligament repair involves stitching or reattaching the torn ligament directly if the tissue is still intact enough to heal. This is more commonly used for certain ligaments like the MCL or LCL when the tear is near the attachment site. A ligament reconstruction involves replacing the damaged ligament with a graft (usually a tendon from your own body or from a donor). This is often required for ACL and more complex or chronic injuries.
How long is the recovery time after ACL or multiligament knee surgery?
Recovery time varies depending on the number of ligaments involved and the type of reconstruction performed. In general:
- Isolated ACL reconstruction: Return to sport may be possible from 9 to 12 months.
- Multiligament surgery (ACL + PCL, LCL or MCL): Recovery may extend beyond 12 months, with early rehabilitation focusing on protection and gradual mobility.
Dr Awwad will tailor your rehabilitation plan to your surgery and functional goals.
What kind of grafts are used for ACL reconstruction?
Dr Awwad uses several graft options depending on your age, activity level, and specific needs:
- Hamstring tendon autograft (commonly used)
- Quadriceps tendon autograft
- Patellar tendon autograft
- Allograft (donor tissue, generally used in revision or multiligament cases)
Each graft has benefits and considerations, which will be explained during your surgical planning.
Will I need a brace after surgery?
No, in most cases a brace is not required after isolated ACL surgery, however may be required if other structures or ligaments are injured. The type of brace and duration of use will depend on the number and type of ligaments repaired or reconstructed.
When can I return to work or sport?
Video: https://drgeorgeawwad.com.au/video/when-can-i-return-to-sport-after-my-acl-injury/
- Desk-based work: Often possible within 2–4 weeks, depending on your mobility and commute.
- Manual or physically demanding work: Usually requires 3–6 months or more.
- Contact or pivoting sports: A full return may require 9–12+ months, with clearance based on functional testing.
Can a torn ligament heal without surgery?
Some ligament injuries, such as low-grade MCL sprains or partial LCL tears, may heal with non-surgical treatment, including rest, bracing, and physiotherapy. ACL tears, especially in active individuals or those with knee instability, typically require reconstruction for long-term stability.
Is ACL surgery urgent?
ACL reconstruction is not typically an emergency. However, delaying surgery in active individuals or those with knee instability may increase the risk of further damage to cartilage or menisci. Dr Awwad will advise on timing based on your symptoms and goals.
Will I be able to kneel or squat after surgery?
Kneeling or squatting may be uncomfortable in the early stages but often improves with rehabilitation. Some graft types (e.g. patellar tendon) may cause longer-lasting discomfort during kneeling. Your physiotherapy plan will include gradual reintroduction to these activities.
Will I need physiotherapy after surgery?
Yes. Rehabilitation is critical to restoring strength, flexibility, and neuromuscular control after ligament surgery. Dr Awwad works closely with physiotherapists and provides detailed protocols to support each phase of your recovery.
What happens if I re-injure the same ligament?
If a reconstructed ligament fails, whether due to trauma, early return to sport, or graft-related issues, revision surgery may be needed. This involves more complex planning, but Dr Awwad has experience managing both primary and revision ligament reconstructions.
Download PDF Rehabilitation Guidelines
ACL Procedures
- ACL Reconstruction
- ACL & MCL Reconstruction and Rehabilitation
- ACL & PCL Reconstruction
- ACL, LCL, Posterolateral Corner Reconstruction
- ACL Reconstruction & Meniscal Repair
- ACL Reconstruction & Meniscal Root Repair
- ACL Tibial Avulsion Fracture Repair
PCL Procedures
- PCL Rehabilitation Protocol
- Non-Operative PCL Protocol
- PCL & Meniscal Root Repair
- PCL, ACL, LCL, Posterolateral Corner Repair
LCL / MCL Procedures
- LCL Reconstruction
