Debridement and Synovectomy
Relieving joint pain through debridement and synovectomy surgical procedures
Debridement and synovectomy are two surgical procedures that may be used to treat joint pain, swelling, and restricted movement caused by damaged or inflamed tissue. These procedures are typically performed arthroscopically and may help relieve symptoms in patients with chronic joint inflammation, early-stage arthritis, or mechanical irritation from loose or damaged tissue within the joint.
Dr George Awwad may recommend debridement or synovectomy as part of a joint preservation strategy, either alone or in combination with other procedures such as meniscal repair or cartilage treatment. This page outlines what each procedure involves, who may benefit, and what to expect during recovery.
What is joint debridement?
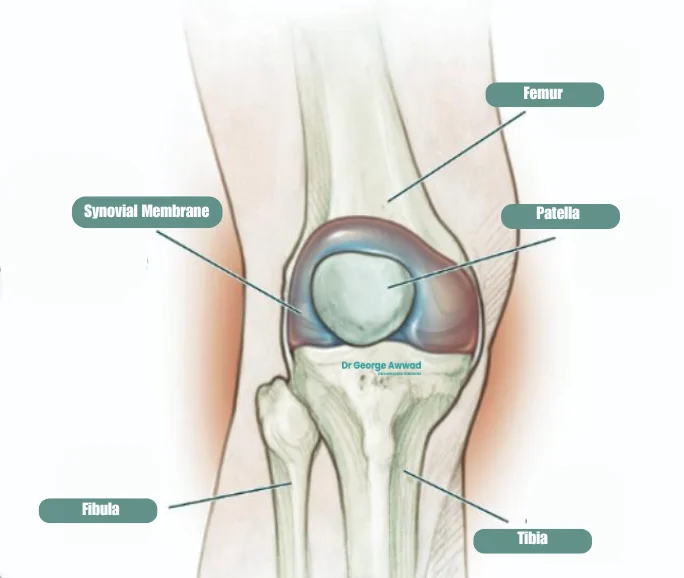
Joint debridement is a surgical procedure that involves the careful removal of damaged, inflamed, or loose tissue from within the knee joint. This may include fragments of cartilage, bone spurs, inflamed synovial tissue, scar tissue or other debris that is interfering with the smooth movement of the joint.
The goal of joint debridement is to reduce pain and improve joint function. It is typically performed using a minimally invasive technique called arthroscopy, which involves inserting a small camera and specialised instruments through tiny incisions around the knee.
During the procedure, Dr George Awwad visually inspects the inside of the joint, identifies any areas of damage or inflammation, and removes or smooths the affected tissue. This may help restore more natural movement and reduce mechanical irritation caused by loose or rough joint surfaces.
As with all procedures, Dr Awwad carefully evaluates your condition and imaging studies to determine if debridement may play a role in your broader treatment plan.
What is a synovectomy?
A synovectomy is a surgical procedure that involves removing part, or all of the synovium, the thin lining of tissue that surrounds and lubricates the knee joint. The synovium normally produces fluid that helps the joint move smoothly. In some conditions however, such as rheumatoid arthritis, inflammatory arthritis, or chronic synovitis after injury, this tissue can become inflamed and thickened.
When the synovium remains inflamed despite medications and other non-surgical measures, it may cause ongoing pain, swelling, stiffness, and reduced mobility in the knee. A synovectomy may be recommended to relieve symptoms, protect the joint from further damage, and help improve function. The procedure is often performed using minimally invasive arthroscopy, where small instruments and a camera are inserted through tiny incisions in the knee. This approach typically allows for a shorter recovery time compared to open surgery. In some more complex cases, an open synovectomy may be required for complete removal of the diseased tissue.
Dr George Awwad carefully assesses each patient’s condition to determine whether synovectomy may be beneficial, taking into account the underlying cause of synovial inflammation, the extent of joint damage, and overall health factors.
What conditions can be treated with debridement or synovectomy?
Joint debridement and synovectomy are orthopaedic procedures that may be recommended to relieve pain, reduce swelling, and improve joint function in a range of inflammatory or degenerative joint conditions. These procedures are typically performed arthroscopically (via keyhole surgery) and can offer a minimally invasive approach to managing chronic or recurrent symptoms that have not responded to non-surgical treatments such as medications or physiotherapy.
Osteoarthritis (OA)
- Debride loose cartilage flaps causing locking
- Removing loose bodies (fragments of bone or cartilage) that become stuck in the joint
Inflammatory Arthritis (e.g. Rheumatoid Arthritis)
- Persistent joint pain and swelling
- Stiffness and loss of range of motion
- Progressive joint damage over time
A synovectomy may be considered to remove the inflamed synovial tissue, particularly if the disease is affecting one or two joints and is not well-controlled with medications. This may help reduce symptoms and slow the progression of joint damage.
Pigmented Villonodular Synovitis (PVNS) and Synovial Chondromatosis
- PVNS involves the abnormal overgrowth of pigmented synovial tissue, which may damage cartilage and bone.
- Synovial chondromatosis causes the formation of cartilage nodules within the joint lining, which may become loose and lead to pain, swelling, or locking.
Both conditions may be managed surgically through arthroscopic or open synovectomy, sometimes combined with debridement or removal of loose bodies.
Septic Arthritis (Infection)
- Clear out infected or necrotic material
- Reduce bacterial load
- Improve joint movement
Post-Traumatic Synovitis or Loose Bodies
- Removing these loose bodies or scar tissue
- Reducing inflammation
- Helping restore smoother movement of the joint
Tailored Treatment for Each Condition
Not all patients with these conditions will require debridement or synovectomy. During your consultation, Dr George Awwad will perform a thorough clinical assessment, review your imaging, and discuss whether surgical treatment may be appropriate based on:
- The severity and type of joint damage
- Your age, activity level, and goals
- Your response to previous non-surgical treatments
When might debridement or synovectomy be recommended?
Joint debridement or synovectomy surgery may be considered when non-surgical treatments such as rest, anti-inflammatory medications, corticosteroid injections, or physiotherapy have not provided sufficient relief. These procedures are typically used to address joint pain, swelling, or mechanical symptoms (such as catching or locking) caused by damage or inflammation within the joint.
Dr George Awwad may recommend one or both of these procedures based on the underlying condition, your symptoms, and the severity of joint involvement.
Situations where debridement may be considered:
- Mechanical symptoms due to loose fragments: If cartilage or bone fragments are floating within the joint space and causing catching, locking, or giving way.
- Meniscal or cartilage injury: When damaged soft tissue is causing persistent irritation or obstruction within the joint.
- Post-traumatic joint issues: Following injury, debris or scar tissue may form within the joint and contribute to limited movement or discomfort.
Situations where synovectomy may be considered:
- Inflammatory arthritis: In conditions such as rheumatoid arthritis, psoriatic arthritis, or lupus, thickened and inflamed synovial tissue may be removed to reduce pain and prevent further joint damage.
- Recurrent joint swelling: If chronic synovitis (persistent joint lining inflammation) continues despite medical treatment.
- PVNS (Pigmented Villonodular Synovitis): To remove diseased synovial tissue and reduce recurrence risk.
- Synovial chondromatosis: When cartilage nodules form within the synovium and interfere with joint movement.
- Infection control: As part of treatment for joint infections (septic arthritis) to remove infected tissue and reduce bacterial load.
Individualised Assessment
- Carefully assess your symptoms and clinical history
- Review imaging such as X-rays or MRI scans
- Consider your overall joint function, level of inflammation, and long-term goals
If surgery is considered appropriate, Dr Awwad will explain the procedure in detail, discuss the potential risks and benefits, and provide you with a tailored treatment and recovery plan.
Who may not be suitable for these procedures?
Patients with advanced osteoarthritis
Limited benefit in longstanding symptoms
Individuals with low inflammatory burden
Patients with significant joint instability
Medical conditions that increase surgical risk
Patients with certain medical conditions may not be suitable candidates for elective arthroscopic surgery, including:
- Poorly controlled diabetes or heart disease
- Bleeding disorders
- Active infection
- Immunosuppression
- Inability to safely undergo anaesthesia
Personalised Assessment Is Essential
Arthroscopic vs open technique: how are these surgeries performed?
Arthroscopic technique (minimally invasive surgery)
- Small incisions (portals) are made to access the joint.
- Sterile fluid is introduced to expand the joint and improve visibility.
- A fibre-optic camera projects images of the joint interior onto a screen.
- Smaller incisions and minimal scarring
- Reduced post-operative pain
- Shorter hospital stay
- Faster recovery and return to activity
Open technique (traditional surgery)
- There is extensive joint damage
- Arthroscopy cannot reach certain areas
- Open exposure is needed for more precise removal of abnormal tissue
- A longer incision is made over the joint
- The joint is carefully opened to expose the damaged or inflamed structures
- The surgeon directly removes the affected tissue under direct visualisation
Which technique is used in your case?
What are the goals of debridement and synovectomy surgery?
1. Reduce pain and inflammation
- Loose bone or cartilage fragments
- Inflamed synovial tissue (as seen in inflammatory arthritis or PVNS)
- Scar tissue
2. Improve joint movement and function
- Restore smoother movement
- Improve joint flexibility and range of motion
- Enhance daily functional activities such as walking, bending, or lifting
3. Slow the progression of joint damage
- Reduce further cartilage wear
- Control localised inflammation
- Delay the need for more invasive procedures such as joint replacement
4. Improve quality of life
- Increased mobility
- Improved ability to participate in daily and recreational activities
- Better sleep and overall wellbeing
5. Diagnose and guide further treatment
Debridement and synovectomy as part of a joint preservation plan
Joint preservation refers to a treatment approach aimed at maintaining the health and function of a natural joint for as long as possible, particularly in younger or active patients who may wish to delay or avoid joint replacement surgery. In this context, debridement and synovectomy procedures may play a valuable role.
Preserving joint structure and delaying degeneration
Both debridement and synovectomy can be used strategically to manage early or moderate joint damage before more extensive structural changes occur. By addressing mechanical or inflammatory contributors to pain and dysfunction, such as loose bodies or chronic synovial inflammation, these procedures may help:
- Minimise ongoing joint surface damage
- Improve biomechanics and reduce stress on remaining cartilage
- Delay the progression of osteoarthritis
Complementary to other joint-preserving strategies
- Weight management and exercise: to reduce joint load and maintain muscle strength
- Physiotherapy: to support mobility and optimise function
- Injection therapies: such as corticosteroids or hyaluronic acid, to reduce inflammation and support joint lubrication
- Correction of biomechanical issues: through orthotics or bracing
- Realignment procedures: in some cases, a knee osteotomy or other surgical realignment may be recommended in combination to redistribute weight-bearing forces across the joint
- Concurrent management with rheumatologist: in patients with inflammatory conditions
Patient selection is key
What is the recovery process after surgery?
Hospital stay and immediate post-operative period
- A padded dressing or compression bandage around the joint
- Instructions on how to manage pain and swelling (e.g. ice packs, elevation, medication)
- Guidance on how much weight you can place through the joint (some patients may require crutches or a walker for a short time)
Wound care and follow-up
- Keeping the wounds clean and dry
- Watching for signs of infection such as redness, discharge, or fever
- Attending a follow-up appointment with Dr Awwad (usually within 1–2 weeks)
Rehabilitation and physiotherapy
- Restore joint range of motion
- Improve strength and stability
- Support return to daily activities and work
Returning to daily activities and work
- Desk-based or sedentary work: Many patients return within 1–2 weeks
- Light physical work: May require 2–4 weeks off
- Heavy manual labour or high-impact activity: May need 6 weeks or longer before returning, based on recovery progress
