Knee Fracture Surgery
Surgical treatment for fractures of the knee joint
Knee fractures are serious injuries that involve a break in one or more of the bones that make up the knee joint, most commonly the patella (kneecap), distal femur (thighbone), or proximal tibia (shinbone). These injuries are often the result of high-impact trauma, falls, or sporting accidents, and may affect not only the bone but also nearby cartilage, ligaments, and soft tissues.
Knee fracture surgery may be recommended to restore joint stability, preserve function, and support long-term mobility. Treatment typically involves realigning the broken bone fragments and securing them with internal fixation devices such as plates, screws, or rods. Early and accurate surgical intervention aims to reduce the risk of complications such as stiffness, arthritis, or prolonged disability.
On this page, you’ll find detailed information about the types of knee fractures, when surgery may be required, the procedures involved, and what to expect during recovery. Dr George Awwad will guide you through each step of your care, tailoring your treatment to your individual injury and functional goals.
What are the different types of knee fractures?
Patella (kneecap) fractures
The patella is a small, triangular bone that sits at the front of your knee. It protects the joint and helps your quadriceps muscle extend the leg. A patellar fracture usually results from a direct blow to the knee such as a fall or collision and may involve a clean break or a shattered bone. These fractures can be displaced (the bone fragments are separated) or non-displaced (the bone remains aligned).
Distal femur fractures (lower end of the thigh bone)
The distal femur is the lower part of the thigh bone that connects to the top of the knee joint. Fractures in this area often occur from high-energy trauma (like motor vehicle accidents) or low-energy injuries in older adults with osteoporosis. These fractures can extend into the knee joint, potentially damaging cartilage and causing long-term joint issues if not treated properly.
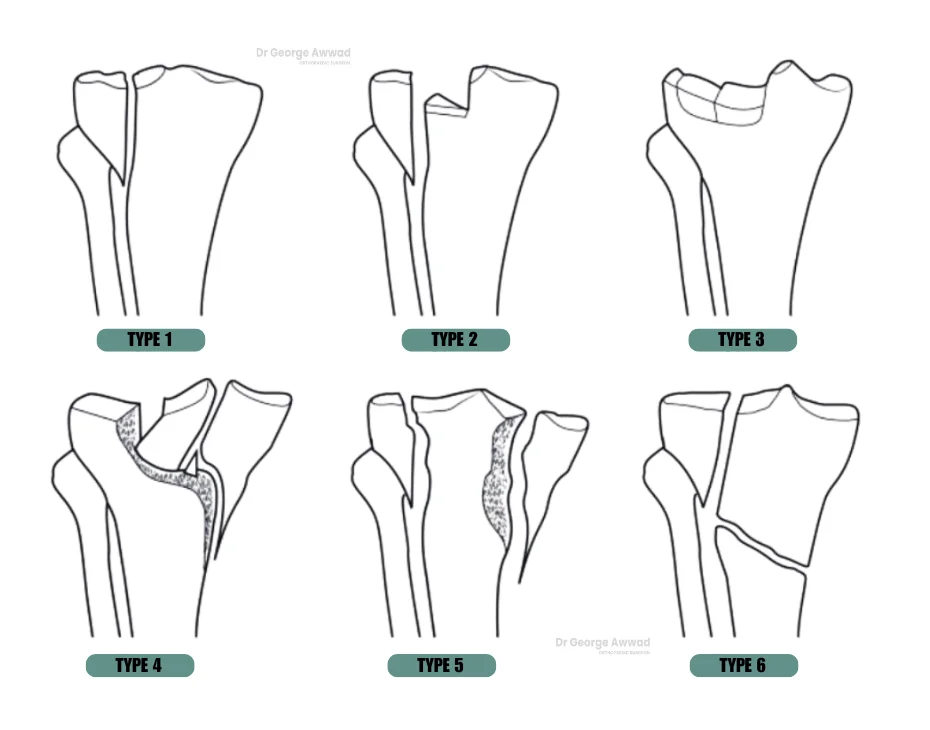
Proximal tibia fractures (upper end of the shin bone)
The proximal tibia forms the lower part of the knee joint and supports much of your body weight. Fractures here are sometimes called tibial plateau fractures and can affect the stability and alignment of the knee. These injuries are often seen in sports injuries or falls and may be associated with ligament or meniscal damage due to the force required to fracture this strong bone.
Tibial spine fractures
Segond fractures
Multiple and complex knee fractures
Some patients may experience fractures involving more than one bone in the knee, or multiple fracture lines within the same bone. These are often classified as complex or comminuted fractures and require a tailored surgical approach to restore joint anatomy and function.
Understanding your specific type of fracture is the first step in developing a treatment plan tailored to your injury. During your consultation, Dr George Awwad will review your imaging and explain the type of fracture you have, how it affects your joint, and which treatment option is most appropriate for your recovery.
Causes and risk factors for knee fractures
Multiple and complex knee fractures
1. High-impact trauma
2. Preoperative Planning
3. Falls and slips
4. Twisting or rotational force
5. Direct impact or blunt force trauma
Risk factors that increase the likelihood of a knee fracture
1. Osteoporosis and low bone density
2. Age
3. Participation in high-risk activities
4. Previous knee injuries
5. Certain medical conditions
Symptoms of a fractured knee
Pain and tenderness
Swelling and bruising
Inability to bear weight
Reduced range of motion
Visible deformity
Grinding or clicking sensation
Numbness or tingling
How are knee fractures diagnosed?
Medical history and clinical examination
- Local swelling, bruising, or deformity
- Tenderness over the bones or joint
- Range of motion and joint stability
- Circulation, sensation, and muscle strength in the leg and foot
X-rays (Radiographs)
Standard X-rays are usually the first step in confirming the presence of a fracture. They help visualise the bone structure, alignment, and whether the break is:
- Displaced or non-displaced
- Simple or comminuted (multiple fragments)
- Intra-articular (extending into the knee joint)
CT scan (Computed Tomography)
MRI (Magnetic Resonance Imaging)
Additional tests if required
When is surgery typically recommended for a knee fracture?
Surgery is typically recommended for knee fractures when the broken bone is displaced, unstable, or involves the joint surface in a way that may affect long-term knee function. Dr George Awwad carefully assesses the type of fracture, your overall health, activity level, and the risk of complications before recommending surgical treatment.
Common reasons for surgical intervention
- Displaced fractures: If the bone fragments have moved out of alignment, surgical fixation is often needed to restore the correct anatomy.
- Intra-articular fractures: When the break extends into the knee joint (such as a tibial plateau fracture), surgery helps ensure joint congruency to reduce the risk of arthritis.
- Unstable fractures: Some fractures are inherently unstable due to muscle and ligament forces pulling on the bone, making non-operative treatment difficult.
- Multiple fragments (comminuted fractures): Surgery can help reassemble and stabilise complex fracture patterns.
- Open fractures: If the bone has broken through the skin, urgent surgery is required to clean the wound and fix the fracture to reduce infection risk.
- Failure of non-operative management: If a fracture does not heal as expected with bracing or casting, surgery may become necessary.
Surgical goals
The main goals of surgery are to:
- Realign the fractured bones (known as reduction)
- Secure them with implants such as plates, screws, or rods
- Restore the joint surface, if involved
- Support early movement to reduce stiffness and promote recovery
Types of surgical procedures used to treat knee fractures
Open reduction and internal fixation (ORIF)
Intramedullary nailing
Patella tension band wiring or screw fixation
External fixation
Arthroscopically assisted fixation
What happens during knee fracture surgical procedure?
Before surgery
- Imaging: X-rays and often a CT scan are used to understand the exact fracture pattern.
- Pre-operative planning: Dr Awwad will create a surgical plan based on your injury, overall health, and activity level.
- Anaesthesia: The procedure is typically performed under general anaesthetic or regional (spinal) anaesthesia.
Advanced, multi-compartment arthritis
Severe stiffness or limited range of motion
Inflammatory arthritis or systemic joint disease
Poor bone quality
Unrealistic expectations
After surgery
- You will be monitored in the recovery unit before returning to the ward.
- Pain management and early movement strategies will begin under the guidance of Dr Awwad and the physiotherapy team.
- You may be advised to avoid putting weight on the leg for a period, depending on the stability of the repair and the healing progress.
What is the recovery process like after knee fracture surgery
Hospital stay and immediate post-operative care
- Most patients stay in hospital for 1 to 3 days, depending on the complexity of the surgery and initial mobility.
- Pain and swelling are managed with prescribed medications and supportive measures like elevation and ice.
- A brace, splint, or cast may be used to protect the knee and limit motion while the bone heals.
Weight-bearing and mobility
- Whether you can put weight on your leg immediately after surgery depends on the type and stability of the fracture.
- Dr Awwad will provide specific guidance—some patients may need to remain non-weight-bearing for several weeks, while others may begin partial or full weight-bearing earlier.
- Crutches or a walking frame are often used initially to support mobility and safety.
Physiotherapy and rehabilitation
- A physiotherapy program typically begins during your hospital stay and continues after discharge.
- Early exercises may focus on:
- Maintaining range of motion in the hip, ankle, and unaffected joints
- Gentle knee mobilisation (as permitted)
- Muscle activation and strengthening
- Over time, the program will progress to:
- Weight-bearing exercises
- Balance and coordination retraining
- Functional activities such as walking, climbing stairs, and returning to sport (if applicable)
Bone healing and imaging follow-up
- X-rays are taken periodically to monitor how well the fracture is healing.
- It can take around 6 to 12 weeks for the bone to unite, although this varies based on the fracture type and patient factors.
- Full recovery may take several months, especially in more complex or intra-articular fractures.
Returning to daily activities
- Driving: You may return to driving once you can fully bear weight, safely control the pedals, and are no longer taking strong pain medication. This is typically around 6–8 weeks but may vary.
- Work: Office-based jobs may be resumed in 2–6 weeks, while physically demanding roles may require 3 months or longer.
- Sport: High-impact activities and sports are usually delayed for at least 4–6 months to reduce the risk of re-injury.
Ongoing care with Dr Awwad
Potential risks or complications of knee fracture surgery
1. Infection
- Post-operative infection may occur at the skin incision or around the implanted hardware.
- This is generally minimised through sterile techniques and may be treated with antibiotics if detected early.
- In rare cases, a deep infection may require additional surgery.
2. Blood clots (Deep Vein Thrombosis or Pulmonary Embolism)
- Surgery and reduced mobility increase the risk of blood clots forming in the leg veins.
- Preventive measures may include blood-thinning medication, compression stockings, and early mobilisation.
3. Delayed bone healing or nonunion
- Some fractures may take longer than expected to heal, particularly in patients who smoke or have certain medical conditions.
- In rare cases, the bone may not heal at all (nonunion), which could require further surgical intervention.
4. Malunion
- This occurs when the fracture heals in an incorrect position, which may affect joint alignment or function.
- In some cases, revision surgery may be needed to restore optimal alignment.
5. Implant-related issues
- Plates, screws, or other fixation devices are commonly used to stabilise the fracture.
- These implants can sometimes cause irritation, loosening, or may need removal after the bone has healed.
6. Joint stiffness or reduced range of motion
- Scar tissue or prolonged immobilisation can result in knee stiffness.
- Physiotherapy is important to help restore joint mobility and minimise long-term stiffness.
7. Post-traumatic arthritis
- Damage to the cartilage or joint surface during the fracture can increase the risk of developing osteoarthritis in the future.
- In some cases, joint replacement surgery may be needed later in life.
8. Nerve or blood vessel injury
- Although rare, surrounding nerves or blood vessels may be injured during the fracture or surgery, which can cause numbness, weakness, or circulation issues.
9. Persistent pain or swelling
- Some patients may experience ongoing discomfort, even after the fracture has healed, especially if there is residual soft tissue damage or early arthritis.
10. Anaesthesia-related risks
- These include rare but possible complications such as allergic reactions or respiratory issues, which are managed by your anaesthetic team.
Knee Fracture Surgery FAQs
Can I go private for my knee fracture surgery?
How long does it take to recover from knee fracture surgery?
Will I need physiotherapy after surgery?
Can metal plates or screws stay in the body permanently?
When can I return to work or driving after surgery?
This depends on the type of surgery, your occupation, and whether your driving leg is affected.
- Office-based work: often possible within 2 to 6 weeks.
- Manual or physical jobs: may require 8 to 12 weeks or longer.
- Driving: typically allowed once you are no longer using crutches and can safely control the vehicle — usually after 6 to 8 weeks. Dr Awwad will provide individual guidance based on your recovery.
Is knee fracture surgery painful?
What happens if the bone doesn’t heal properly?
In rare cases, a bone may not heal completely (nonunion) or may heal in a less-than-optimal position (malunion). If this causes pain or functional problems, additional surgery such as revision fixation or corrective osteotomy may be needed.
